The Oscar Puzzle
Or, how to disrupt a regulated industry full of scaled incumbents over decades
Welcome to the 1,162 newly Not Boring people who have joined us since last Monday! Join 98,942 smart, curious folks by subscribing here:
🎧 To get this essay straight in your ears: listen on Spotify or Apple Podcasts (soon)
Hi friends 👋,
Happy Thursday!
Today is a first for Not Boring: a Sponsored Deep Dive on a public company, Oscar Health. I’ve only done Sponsored Deep Dives on private companies (and one blockchain), not for any reason other than the fact that startups have been the only ones to reach out. As a reminder, you can read how I choose what companies to write Sponsored Deep Dives on here.
Oscar fits the three things I look for in a Sponsored Deep Dive company:
I believe in the company. Table stakes, but true here. I would invest my own money (although I haven’t yet to avoid that layer of conflict) and I would write about Oscar even if they weren’t paying me (don’t tell Oscar!).
The company has lessons applicable beyond the company itself, and potential benefits to you all. There’s a ton to learn here for anyone interested in taking on regulated, backwards industries with deep-pocketed, scaled incumbents. (Hint: it’s a long, hard road, but doable!)
The company’s story is interesting and fits with the trends we’re all most interested in. I started writing about healthcare a lot more at the end of last year, and it’s one of the complex problems I want to dig into more this year. This decade could be to HealthTech what the past one has been to FinTech.
Beyond those three things, Oscar is a special one. It’s the only health insurance provider I’ve actually chosen for myself (way back in 2013), one of NYC’s most successful startups of the past decade, and my favorite kind of company: one whose complexity means that the market has a hard time understanding it.
That complexity comes from the fact that Oscar is trying to be two things at once: an insurance company and a tech platform. It’s a big bet -- those are two very different businesses -- but if it pays off, they have the chance to make the healthcare experience meaningfully better.
Plus, while it’s no longer private, it’s still very much an underdog in an industry full of giant incumbents, just like a startup. Despite its success, people still assume the giants will hold their positions for decades. Maybe that’s true in insurance in a way that it hasn’t been for any other industry, but that’s not the bet I’d make.
Let me put the disclaimer/disclosure right up front:
Disclaimer/Disclosure: THIS IS NOT INVESTMENT ADVICE! It never is, but that’s particularly true in an industry like insurance in which I’ve spent much less time. This is for educational and entertainment purposes only. Do your own diligence. I decided not to buy any OSCR since I knew I was writing this piece, although I may buy some after sending. This will likely be my stance on public company deep dives going forward. Thrive Capital, a large shareholder in Oscar, is an LP in Not Boring Capital.
And let’s get to it.
The Oscar Puzzle
In late 2013, when I left the cushy confines of Bank of America Merrill Lynch and its gold-plated corporate insurance plan to head to a small Canadian startup that hadn’t even established a US entity, I was given a budget and told to go find my own health insurance. Oddly, I knew exactly what health insurance I wanted to get: Oscar.
I’d seen the ads on the subways: “Hi, we’re Oscar, a new kind of health insurance company.” I loved the clean look. They used *tech*. I was now in “tech.” They were from New York. I lived in New York. It was a no-brainer.
And when that clean welcome box showed up -- a welcome box! from an insurance company! -- I knew I’d made the right choice.
(I checked with the company, and I was Member #5,540. At Oscar’s current 594,000 members, that means I was in the first 1% of people ever to sign up.)
Little friendly touches like that box were all part of Oscar’s original vision of building a health insurance company that could help its members navigate the healthcare system like a doctor in the family would.
Since I signed up, Oscar has grown membership over 100x. It’s on a multi-billion dollar revenue run rate. It launched a tech platform, +Oscar, and partnered with leading health systems like Cleveland Clinic. It went public… and its stock is getting crushed.
Oscar IPO’d on March 3rd at $39 per share and started trading at $36 per share, good for a market cap just north of $7 billion. Since then, it’s down nearly 77%, its market cap hovering around $1.5 billion.
It’s underperforming both the major indices…
…and the traditional health insurance companies, like UnitedHealth, Cigna, Anthem, and even Humana, whose stock has struggled more than its peers as of late.
On the surface, the mystery is solved simply: Oscar isn’t profitable yet.
Say what you want about the traditional US health insurance industry (OK, fine, twist my arm: it’s confusing, inefficient, expensive, antiquated, and about 20 years behind on UX), but those companies print money. In Q3 2021, UnitedHealth, the most profitable, made $4.1 billion on $72.3 billion in revenue.
Oscar, on the other hand, loses money on every patient on average. In health insurance terms, its combined ratio is greater than 100%. In Q3 2021, Oscar put up an adjusted EBITDA loss of $189 million on $673 million in revenue. Oscar’s stock had started to recover into Q3 earnings, but fell when the company reported that its medical loss ratio (MLR) – the percentage of premium it pays out for care – shot up from 82.4% in Q2 to 99.7% in Q3 thanks to an unfavorable risk adjustment data validation (essentially an insurance payment audit and true-up, read more here if you really want) and, of course, COVID.
Oscar’s membership grew 41% YoY, from 420k to 594k, and revenue grew 63%, but the simple bear case would be that, amending the old joke for health insurance, you can’t lose money on every managed life and make it up in volume.
But still, Oscar is trading below 1x its current revenue run rate, growing very fast, and signing up big partners to its software platform, +Oscar. It feels like an overreaction.
Besides, Oscar wasn’t designed to be profitable yet. In fact, it’s doing two unprofitable things at the same time: building an insurance company and a tech platform from scratch. Both require real scale to become profitable, and Oscar’s bet is that by combining both, they’ll be able to achieve more scale, deliver better care, and generate better margins over the long-term than either side could alone.
That’s why Oscar is making three decades-long, interconnected bets:
Bet #1: Technology can meaningfully improve member engagement, which leads to a better insurance business.
Oscar believes that by building a better experience, it can increase member engagement, by increasing member engagement, it can better guide its members’ care, and that by guiding its members care, it can create better long-term health outcomes at a lower cost.
The pithy way to explain this piece of the strategy is that an ounce of prevention is better than a pound of cure.
Bet #2: A better, tech-powered insurance business will help Oscar sell its technology to hospital systems who want to take risk, improving margins and increasing revenue without increasing Oscar’s risk.
In 2018, Oscar launched what would become +Oscar, its tech platform that lets health systems and other insurers tap into all of the tech that Oscar has built over the past decade.
To understand this piece of the strategy, think Amazon and AWS. Oscar has spent a decade building and battle-testing its own proprietary tech, and now it’s selling that tech to others who need it and earning software margins in the process. Plus, those customers give Oscar scale.
Bet #3: Turning its tech into a platform for third-parties will build scale into both the insurance and tech businesses, which will help improve care and lower costs.
Combining Oscar’s insurance business with its +Oscar partners’ – like the Cleveland Clinic and Montefiore – will give Oscar the scale it needs to build a huge, profitable insurance business. Scale is useful in two ways here:
Insurance Business. More scale means more leverage over the participants in its supply chain, better terms with reinsurers (reinsurance makes up a huge chunk of insurers’ costs), more ability to convince providers to join the network, and a lower admin ratio (amortize administrative costs over more members).
Tech Platform. By opening its tech up as a set of primitives for others in the ecosystem to build with, it will get more data on which types of interventions, digital and physical, work best for which types of patients, and any campaigns it builds for one partner can be copy-pasted and used by any partner, building network effects into the system. More knowledge should lead to better long-term outcomes, and lower costs.
The best way to think about this piece of the business is like Shopify: arming the rebels (in this case, health systems and care providers) in order to compete with the giant incumbent health insurers.
Taken together, it’s a long-term series of bets which is, understandably, confusing to investors in the short-term. As The Abstract Investor summarized, the challenge, and opportunity, is that:
Many tech analysts aren't paying attention to insurance, while insurance analysts won't quite know how to look at a highly tech-stacked insurance company. That presents a potential opportunity for those that can figure out the murky puzzle.
That theory checks out, particularly when you look at how Oscar has performed compared to other public health insurtech companies: Bright Health Group and Clover.
Oscar has traded in-line with those companies despite the fact that the businesses are very different. If you need scale and tech to disrupt health insurance, neither Bright nor Clover has both. Bright is essentially a rollup and partnerships play with little meaningful tech; Clover is a tech player in the Medicare Advantage space with only a quarter of the “lives under management” that Oscar has, and no platform play like +Oscar to achieve scale.
Oscar is the only player in the space that has a shot at achieving scale through technology.
The fact that these three very different companies are trading in line, and falling while the incumbents’ stock prices rise, is weird. It means the market is saying that, unlike practically every other industry in the world, health insurance will be impervious to disruption from technology-first companies. That seems off. I think the Oscar baby is being thrown out with the insurtech bath water.
So today, we’re going to dive in and try to piece together the murky puzzle. I’m not a healthcare analyst, and I don’t even try to play one on the internet, but I do love a good puzzle. We’ll cover:
How Health Insurance Works
Oscar’s Origins: The Hipster Health Insurance
Oscar: A Tech-Enabled Insurance Business
+Oscar: An Insurance-Enabled Tech Platform
Putting Together the Puzzle
To understand the bets that Oscar’s making, we need to understand how health insurance businesses work and where they’re broken. I promise I’ll make it as not boring as possible.
How Health Insurance Works
Almost every industry is easier to understand than it appears at first glance. It’s just about understanding the vocabulary, how businesses make money, and what levers they have to pull. Health insurance, while there’s a ton of complexity in the details, is not hard to understand at a high level.
To understand how US health insurance works at the highest level (conveniently, that’s also the only level at which I understand it), let’s look at three things:
The Size and Composition of the Market
The Health Insurance Profit Formula
The Two Main Reimbursement models
The Size and Composition of the Market
Healthcare in the US is an unimaginably large market.
Americans spend $4 trillion on healthcare per year -- 18% of GDP -- and 75% of that passes through insurance companies. Half of Americans have group, or employer-sponsored, health insurance, 35% have government insurance (Medicaid, Medicare, or Military), 9% are uninsured, and 5.9% have non-group plans. This last group, the individual market, is where Oscar started.

The employer market is the monster here. It’s probably what you’re familiar with. Insurance companies sell plans to your company, and you get to choose from among their plans. In this system, your insurance is tied to your job, and people bounce from insurer to insurer as they move jobs. That means that no one insurer is incentivized to optimize for long-term health, so they optimize for the short-term, which often drives up long-term costs.
No wonder, then, as Oscar CEO Mario Schlosser tweeted last week, employer insurance premiums are super-inflationary (i.e. growing faster than the CPI-based inflation rate). Which, in this economy, is saying something!
(Note: this chart only goes back to 2018, but that famous AEI chart of inflationary v. deflationary industries has hospitals as the most inflationary going back to 1998.)
There’s a bright spot, though, in the individual market. Individual, or Affordable Care Act (ACA), premiums are deflationary. Individual premiums have been growing more slowly than CPI-based inflation since 2018. It’s one data point that letting people choose for themselves each year makes for a more efficient market.
Luckily, the ACA market has been growing, with a 21% increase in enrollments over last year during this year’s open enrollment period (which ends on Saturday in case you still need to enroll!).
This is the part of the market that Oscar has been focused on, for a few reasons:
The ACA opened up a new market when it launched in 2014, and it’s growing fast.
When consumers choose their own insurance, consumer experience matters more.
Individuals can stay with the same plan over their lifetime, regardless of whether they switch jobs, meaning that insurers in the individual market are incentivized to provide the best long-term outcomes at the lowest cost over time.
Simply put: Oscar can make a bigger dent in the individual market, and move upmarket from there.
Whether focused on the individual, employer, Medicare, or Medicaid market, the way that insurance companies turn a profit is roughly the same.
The Health Insurance Profit Formula
For as complex as the US healthcare system is, and I’m going to gloss over a lot of complexity here, the formula for health insurance companies to make money is pretty simple:
Profit = Premiums - (Premiums * Medical Loss Ratio) - (Premium * Admin Ratio)
Members pay monthly premiums to their insurers, and insurers pay out a percentage of those premiums in claims to cover members’ medical expenses (Medical Loss Ratio, or MLR) and another percentage to cover administrative expenses, essentially SG&A (Admin Ratio) . Together, the MLR and Admin Ratio are the Combined Ratio.
There are other things in here – like reinsurance costs and risk adjustments – but I promised not to bore you. Just know those costs come out of direct and assumed policy premiums before getting to the “premiums earned” number that’s used in the ratio calculations.
Anyway, if the Combined Ratio is less than 100%, the insurance company makes money; if it’s more than 100%, it loses money.
Adding just one layer of complexity, the ACA requires insurers to pay out at least 80-85% of premiums in claims (80% for individual and small group insurers and 85% for large group insurers), and then refund any leftover money to members if they don’t.
So the name of the game is to get your MLR as close to 80-85% as possible, and keep administrative costs relatively low. When margins are capped, it’s all about scale.
The Two Main Reimbursement Models
There are two main reimbursement models in healthcare: fee-for-service and value-based care.
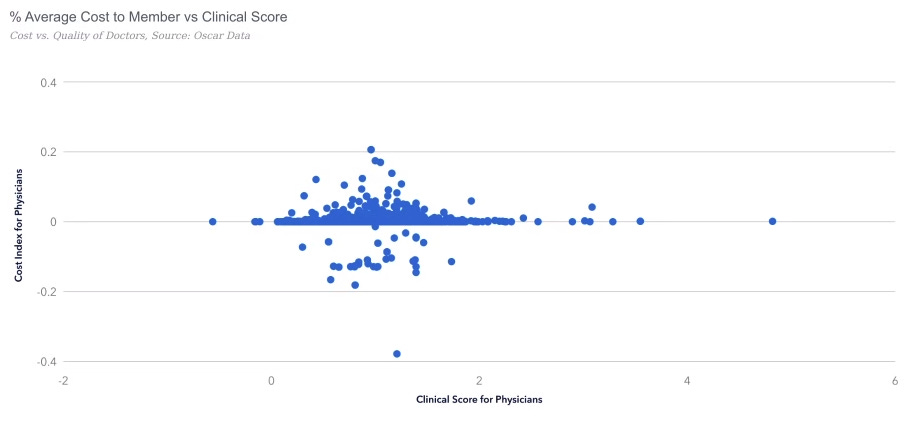
The fee-for-service model is what it sounds like: insurance companies reimburse healthcare providers based on the services that they provide. This incentivizes providers to provide more, and more expensive care. That would be great if more expensive care were correlated with better health outcomes, but it’s not. It’s almost entirely random.
Value-based care, on the other hand, is a form of reimbursement that ties payments to the quality of care provided, and ideally, to the results. This sounds like the ideal system, but in practice, it’s complicated. How do you measure effectiveness? Over what time period? It’s a nightmare.
Coordinating between separate insurance providers and care providers is too complex to really work in practice. Instead, the two sides are beginning to merge.
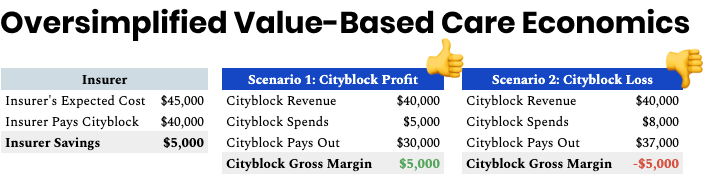
One example is Cityblock Health, which I wrote about last June. The insurer – typically the government in the case of Medicaid – pays them a certain dollar amount per Medicaid patient per year. Cityblock’s job is to keep that patient healthy for less than the government pays them, which mainly comes down to preventing expensive hospital visits. They can do almost anything with that money – from at-home visits to technology to specialist visits – to keep patients healthy for a lower cost. The oversimplified version of their model looks like this:
Why’s it not just about keeping costs low to capture the biggest spread? Two reasons:
Short-term, you need to avoid repeat hospital visits to make money. That means better preventative care.
Cityblock and Oscar want to retain members as long as possible, and therefore generate more margin over time if they keep those patients healthier, and out of the hospital, longer.
Value-based care is the best framework through which to understand Oscar and its two businesses.
Its tech-enabled insurance business, Oscar, says, “We’re taking financial risk for these patients already, let’s use technology and engagement to make sure they get better care, at a more affordable cost, and stay healthier (and out of the hospital) longer.”
Its tech platform, +Oscar, says to care providers, “You’re providing care to these patients anyway, if you provide better care at a lower cost, you should capture that financial upside. Here, use the tools we built to do that.”
Combined, the hope is that the two businesses create enough scale that Oscar is able to drive down its own costs, lower MLRs and admin costs, and allow everyone in the ecosystem to learn from each other, provide better care, and lower costs even further.
So… how does it plan to do that? Let’s go back to the beginning. Hi, Oscar.
Oscar’s Origins: The Hipster Health Insurance
It all started back in 2012, when Josh Kushner, the great, great grandson of the eponymous Oscar, broke his leg and Mario Schlosser, a German living and working in America, found out he and his wife were pregnant. Josh and Mario, Harvard Business School classmates who’d been very successful since, are both really smart. If they couldn’t figure it out, there was a problem.
When they linked up, Mario told Josh he’d been thinking of ways to make US healthcare more efficient, and realized that many of the problems, and opportunities to fix them, stemmed from the health insurers. So Mario (CEO), Josh (now Chairman), and a third HBS classmate, Kevin Nazemi, a former director of healthcare at Microsoft, got to work.
In 2012, they incubated Oscar out of Thrive Capital as a new kind of health insurance company, one that married insurance and technology. At the time, there was no such thing as “Insurtech.” The category wouldn’t even be named for almost four years, but they knew that tech could help.
Mario, Josh, and Kevin had seen how technology was being used to improve all sorts of legacy industries, and realized that they could serve members better, and build a stronger business, if they built their own tech stack from the ground up.
They also saw that the 2010 passage of the Affordable Care Act (“ACA” or “Obamacare”) would mean more consumers choosing their own health insurance.
The Oscar founders correctly predicted the intersection of those two trends:
As the individual market expanded thanks to the ACA, more consumers would be choosing their own insurance provider.
Those consumers would want the types of experiences they were beginning to receive in every other part of their life, from calling a cab to ordering food.
But building a tech company and an insurance company at the same time wouldn’t be easy. In the S-1 that the company filed to go public last year, Mario and Josh wrote of their early decision to make that happen by developing the full tech stack in-house, “We understood it would make the challenge of being a startup health insurer even harder. But we believed it was the only way to create a differentiated member experience.”
As Forbes put it back in 2013, right at the beginning, the Oscar co-founders planned “to change the health insurance industry through technological interfaces, telemedicine and real transparency. Their goal is to redesign insurance to be geared toward the user experience, to make patients seek out their insurer before their doctor.”
That’s a key theme, and one that we’ll come back to: being the first call is key to the model.
The team built for a little over a year, and when the ACA hit New York in 2014, Oscar was there from the first open enrollment. The Wall Street Journal wrote that, “It signed up more than 15,000 people before the March 31 Affordable Care Act open enrollment deadline.” When Oscar launched in New York, it was the first for-profit insurer to enter the individual market in the state in 25 years.
Since then, for such a complex business, both insurance company and tech company, it’s grown relatively smoothly.
It’s expanded from 15,000 members in New York to 594,000 in 497 counties across 19 states.
As of its most recent earnings in Q3 2021, Oscar’s annualized revenue is $2.7 billion… in just a little over seven years since it took in its first premiums. That incredible growth has come despite the fact that Oscar is only the cheapest plan in less than 10% of the markets it serves.
That’s another piece of the thesis playing out: Differentiation means pricing power.
Building that differentiated product experience on top of a new insurance company hasn’t been cheap. Oscar raised $1.6 billion in venture funding as a private company, and another $1.4 billion when it went public in March.
For 2021, Oscar expects to lose somewhere between $450 and $480 million on an Adjusted EBITDA basis, adding $100 million to expected losses since Q2 estimates after a worse-than-expected medical loss ratio in Q3.
Building an insurance company is hard and capital intensive. Rebuilding a new tech stack from the ground up is hard and capital intensive. Doing both at the same time is doubly hard and doubly expensive.
Part of the bull case for Oscar is that it’s done a lot of the hardest, most expensive work. It’s still building, and it has an insurance business to run, but it’s entered the scaling phase.
Today, whether you’re bullish on Oscar or not comes down to whether you believe the core thesis: that the tech it’s built fundamentally improves the insurance business.
Oscar: The Tech-Enabled Insurance Business
The main idea behind Oscar is that by increasing member engagement, building trust, and being a member’s first call when seeking healthcare, it can run more of healthcare through its own tools -- virtual primary care, virtual urgent care, care routing, and more. Oscar can get you the right care, at the right time, and then wrap plans around that care.
“If you follow the plan,” Mario told me, “we can save you money and save us money.”
Easier said than done. Nobody calls their insurance provider first when they need care. Gun to my head, I’m not sure I could tell you who my insurance provider even is. To get consumers to engage with Oscar like they’d engage with any other best-in-class consumer product, they need to have a best-in-class consumer product. It’s why Oscar had to build everything from the ground up. It had to combine a bunch of different pieces into one, seamless package.
Jim Barksdale famously said, “There are only two ways I know of to make money: bundling and unbundling.” It’s rare to see one company do both.
The first part of Oscar’s master plan, which it’s been executing on for the past decade, is to bundle a bunch of things that other companies offer as point solutions into one seamless health insurance plan:
Custom-Built Provider Networks
Plans
Member Engagement: Digital Experience and Care Teams
Virtual Primary Care & Virtual Urgent Care
Claims Management
Remember, the point of all of this is to provide better care at a lower cost, since Oscar is on the hook for paying care costs out of its premiums. Let’s go over each briefly.
Provider Networks. In every market it enters, Oscar builds out its own provider network: hospitals and doctors that accept Oscar insurance plans. They build around healthcare systems and then add in independent providers as needed. In New York City, for example, Mario told me that they have about 20k of the 40k providers in-network. The company uses the data that it has as a health insurer to pick providers based on a combination of quality, affordability, and other factors.
Plans. Oscar’s bread and butter is serving individuals, who make up about 6% of the market nationally.
Oscar offers them plans that conform to the ACA metal categories: Bronze, Silver, Gold, and Platinum. Finding a plan is dead simple. Enter your age and zip code, click see plans, and get a list of plans by category laid out cleanly. Check it out:
You’ve had to pick healthcare plans before. It’s never this simple or straightforward.
Oscar competes on experience, not price. It rarely offers the cheapest premiums in the markets it serves; it doesn’t try to. In fact, in the roadshow video the company made heading into its IPO, Josh pointed out that Oscar has been growing despite only being the cheapest plan in less than 10% of its markets. In 2022, it’s only going to be the cheapest plan in 5% of its markets. Recall the Health Insurance Profit Formula; higher premiums give Oscar more room to pay more for great care. That great care upfront should lead to lower costs over time.
Despite the higher price, the better experience attracts customers. Typically, Oscar launches in a market with 7-8% market share, and grows to 15% by year three.
Over the past three years, Oscar has begun expanding its addressable market to serve small groups (companies with fewer than 50 employees) and Medicare Advantage (people over 65 can purchase their own healthcare with government money), largely through +Oscar partnerships. We’ll cover these below.
All told, Oscar’s total addressable market in these three categories alone is roughly $450 billion in premiums. There’s a lot of room to run.
Member Engagement
In value-based care, it’s all about being the first call. Being the first call lets Oscar route members to cost-effective options, collect valuable data, and manage their care more comprehensively.
To that end, Oscar members have access to an app and website through which they can find doctors, schedule appointments, manage prescriptions, and complete appointment follow-ups. Through a partnership with Capsule, members can see what drugs will cost ahead of time, and get their prescriptions fulfilled online. They can sort providers by rankings, read reviews from other members, and book online. This feels like what you’d expect from any tech company, but for an insurer, it’s a dramatic step up from the status quo.
When someone signs up for Oscar, they get assigned a Care Team -- six people, including a Registered Nurse, who serve as their consistent points of contact within Oscar. Care Teams can help members understand their plans and what’s covered, find in-network doctors and specialists, tackle their appointment follow-ups, and more, all powered by Rosco, the back-end system Oscar built for its Care Teams.
In Rosco, Care Teams can securely access behavioral and claims data, appointments that members have booked through Oscar, and all of the communications they’ve had with Oscar. Care Teams have access to a more powerful care routing tool than is available on the member-facing site, and can recommend providers based on availability, quality, and cost.
Because Oscar is the insurer, it has cost data in its claims system on each provider and location, so Care Teams can often provide an estimate of what a visit or procedure will cost ahead of time, removing the always-harrowing element of surprise from healthcare. In the future, Mario told me that they should be able to expose cost estimates on the member-facing site in real-time, and pay the doctor in real-time instead of waiting months for claims.
If the Oscar model is all about the engagement, then the proof of its success or failure is in its engagement metrics:
68% of members trust Oscar to advise them on how and where to get care
75% of members use Oscar’s Care Router tool, and ⅔ choose a recommended provider
People who do choose a recommended provider end up saving 7% on average
90% of Oscar members recommend the doctors they found through Oscar
Oscar has an NPS of 40, compared to an health insurer average of 3, according to Forrester Research.
It’s worth pointing out that Oscar does have a slew of negative reviews on the Better Business Bureau site, among others. That was worrying… until I read reviews on its competitors. Turns out, people don’t really leave positive reviews about health insurance companies! On the flip side, LendingTree’s Value Penguin did give Oscar a 4.5/5 stars, higher than any of its competitors.
Virtual Primary Care and Virtual Urgent Care
From the beginning, Oscar has offered virtual primary care as part of its arsenal, starting way back in 2014 with a partnership with TelaDoc, before telemedicine was really a thing. Ahead of the trend once again.
The logic for the combination of telemedicine plus insurance is simple:
Telemedicine appointments are cheaper and more efficient than in-person visits.
They’re more convenient, so people will use them more when they don’t feel well.
More frequent touchpoints mean that Oscar can detect problems earlier, route care, and avoid expensive catastrophes.
Today, Oscar offers its own virtual care, both primary care and urgent care, through doctors employed by the Oscar Medical Group. Virtual visits and messaging with doctors are both free to members, and most of what the doctor recommends in the virtual care session is free to members, too.
For virtual urgent care, members can get connected with a virtual care provider (VCP) 24/7, instantly. Oscar can handle a large chunk of urgent cases virtually, avoiding expensive and lengthy trips to the hospital, saving its members and itself money. When in-person care really is needed, Oscar can help coordinate it.
Plus, for virtual and primary urgent care, the VCP can put formally configured follow-up steps right in your Oscar account, and your Care Team can help guide you through all the steps.
Finally, if you don’t complete any of the follow-ups, you’ll receive automated reminders from the Care Team and get assistance if you need it. They can even incentivize you to do things like fill prescriptions with enticements like Amazon Gift Cards.
All of this comes down to value-based care: since Oscar is on the hook for members’ costs, it’s incentivized to get them the best care in the fastest and most affordable manner, even if that means paying them today to do things that will be beneficial tomorrow.
Campaigns
The most mind-blowing part of my interaction with the Oscar team was when Mario jumped into the system to show me the campaign builder, Oscar’s drag-and-drop workflow automation tool that lets the team, and its +Oscar partners, set up and configure population health, intervention, and marketing campaigns. It was mind-blowing for two reasons:
First, I was impressed that Mario was able to hop right in and comfortably navigate the system as the CEO of a $1.6 billion, 2,000+ employee company, which speaks to both the ease of the tool and to Mario’s hands-on approach to leadership.
(To answer another question I had, he hopped into the company’s Periscope and navigated back and forth between a few dashboards to get me detailed answers. That’s different than the way that I’m used to CEOs pulling data: yelling at the data team in a Slack channel.)
Second, I was impressed by the scope and power of the tool.
At any given time, Oscar has hundreds of campaigns going across the company. One that they have going right now, for example, triggers automated outreach from the Care Team if a member measures their blood pressure with a connected monitor and it comes back high. They can link you to a virtual care provider, and if you don’t respond, they can incentivize you with a gift card.
It’s all managed in a visual flow chart -- simple on the front end, but powered by Oscar’s flexible backend infrastructure and data across its hundreds of thousands of members, which allows Oscar to build specific and powerful campaigns across arbitrarily thin segments of the member population, all designed for more engagement, better long-term outcomes, and lower total cost of care. It lets Oscar do things in a customized and individualized way that other health insurers can’t.
Claims
Last but not least, Oscar built its own claims management, adjudication engine, and interfaces in-house.
For members, that ideally means faster claims processing. For providers, it means faster payments. For Oscar, it means less human time spent dealing with faxed claims. It’s an important piece of Oscar’s infrastructure, but it’s not sexy, so we can move on for now. It’ll become more important in a minute.
All told, Oscar has built a natively integrated, value-based health insurance company that boosts engagement, and by doing so, lets Oscar control costs and improve outcomes over time.
That was a major investment in technology to serve just one insurer that serves just 0.16% of the country’s insured population, though… kind of like Amazon’s servers and all of the custom tooling they built around them were a bit much for one ecommerce company.
So if at this point you believe that the tech Oscar’s built fundamentally improves the insurance business, the mega-bull case is that hospital systems, care providers, and even other insurers will believe it too, enough to adopt +Oscar for themselves.
The second part of the master plan is to unbundle everything they’ve built and offer it to others in the healthcare system as a flexible, modular tech platform.
+Oscar: The Insurance-Enabled Tech Platform
The big trend behind Oscar’s success in the insurance business was the move towards the individualization and consumerization of healthcare, triggered by the ACA. They nailed that one and rode it to a $7+ billion IPO.
Now, there’s another trend happening in healthcare more broadly that Oscar is perfectly suited to power, and capture: the shift towards value-based care and increased risk sharing with the hospital systems and providers themselves.
On a long enough time horizon, everyone wants to become a subscription business, and hospital systems are no different. Instead of relying solely on the fee-for-service model, hospital systems are beginning to move towards a model in which they take the risk, and keep the rewards. It’s healthcare’s own shift from labor to capital that we’re seeing everywhere else in the market.
In other words, everyone wants to be Kaiser Permanente.
I gotta admit, when the movie came out, I thought that Kaiser Permanente was an agriculture company. Turns out, it’s an integrated managed care consortium made up of for-profit and non-profit entities that operates the full stack of healthcare services, from insurance to hospitals to ambulances to physician networks. It has 12.5 million members, and in Q2 2021, it brought in $3 billion in profits.
Today, more health systems want to be like Kaiser Permanente, offering their own insurance plans to patients and shifting to a value-based care model that better aligns them with their patients’ outcomes and gives them more control over their own destiny.
But, as you might have picked up from the last section, building out a modern insurance company is a lot of work and takes the technical and design chops that most healthcare systems don’t have in-house, and probably couldn’t even hire in this environment.
So in 2018, in partnership with the prestigious Cleveland Clinic, Oscar launched what would become +Oscar, its tech platform for health systems and other insurers. +Oscar takes everything that Oscar has built over the past decade -- the risk engine and payment engine, virtual care delivery, population health management, campaign management, Care Teams, and engagement tools -- and delivers it as a set of APIs and services to partners.
“No health insurance company can grow by itself to cover all 350 million Americans,” Josh explained, “it would be impossible to scale because of the licenses, capital reserves, and networks it would require.” It’s equally difficult for hospital systems to become insurers, Josh said. “Building a claims system is hard. Building consumer engagement is really hard. Claims adjudication is really hard.”
So Oscar is attempting to pull off an Amazon and a Shopify at the same time: it’s arming the rebels by offering a set of health insurance primitives that it had to build for itself as first and best customer.
To date, its three biggest partnerships show the breadth of the potential markets it’s able to serve.
Cleveland Clinic + Oscar, the company’s first partnership when it launched in 2018, serves both the individual and group markets. Members get access to the Cleveland Clinic’s network of physicians, nurses, hospitals, and health and wellness centers in addition to Oscar’s apps, Care Teams, virtual care, and fitness incentives. For this partnership, Cleveland Clinic and Oscar split risk 50/50, although future partnerships will likely see Oscar as a software and service provider, and let health systems take all the risk.
Cigna + Oscar is a unique partnership with one of the nation’s biggest large group insurers, Cigna, that lets Oscar serve the small group market. Since selling into small businesses is a different muscle, and requires a more digital approach than large group sales, Cigna partners with Oscar to acquire and serve those members. It also gives Oscar a foot in the door in the small group market.
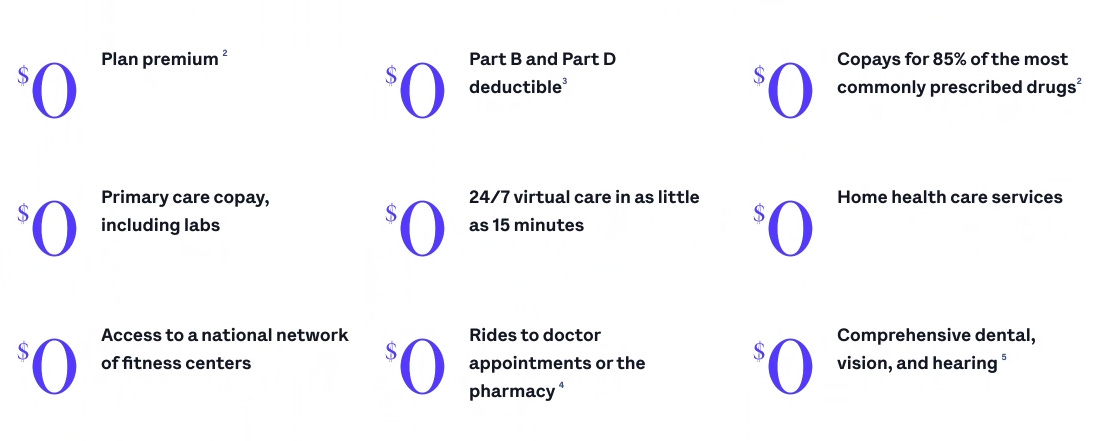
Montefiore + Oscar is a Montefiore-branded Medicare Advantage offering with the large hospital system in the Bronx. Montefiore owned a small insurance company before the partnership, but it wanted a co-branded offering and a way to take more risk on its members, and Oscar wanted a way to access the fast-growing Medicare Advantage market (10k people age into Medicare every day!). The plan is tailor-made for the population it serves, offering things unique to the 65+ population including $0 home health care services and $0 rides to doctors appointments and pharmacies.
The beauty of the Cleveland Clinic and Montefiore partnerships is that they allow the hospital systems to make money for providing better care, not just for providing services. Cleveland Clinic is one of the top medical systems in the country, and Montefiore is one of the top systems serving the Medicare population, and they want to be financially rewarded for that quality without having to rebuild all of the systems that Oscar’s had to over the past decade.
Just this month, Oscar launched HealthFirst +Oscar to go deeper into Medicare Advantage and Medicaid by partnering with the insurer on roughly 60,000 members. The beauty of the HealthFirst and Cigna partnerships is that they allow the insurers to offer their members better service, and allow them to serve members they otherwise may not be able to, while giving Oscar a toehold in large segments of the market – like small group, Medicare, and Medicaid – that it doesn’t serve with its core insurance business.
Like Amazon with AWS (and Lithic), Oscar built tech capabilities for itself, and then realized that other players in the ecosystem would be willing to pay to use their tech in a more modular way. Each partner that works with Oscar can choose to have Oscar power their whole stack, build custom plans, or choose a la carte from the four +Oscar components:
Acquire Risk. This is essentially sales and marketing, which Oscar is well-suited to as a digitally native company. With Montefiore, for example, Oscar powers renewals and recommends plans to members based on their previous usage.
Member Engagement. Partners can white-label Oscar’s digital experience, offer virtual care, and even use its Care Teams to coordinate members’ care. Everything described in the last section can also be made available to +Oscar members.
Campaigning and Campaign Building. Partners can tap into campaigns that Oscar has already run that have proven successful, and can use its campaign builder to create their own. Montefiore members might have very different needs and respond differently to incentives than Cleveland Clinic members, and each can design campaigns, on their own or with Oscar’s guidance, to incentivize actions that lead to better long-term outcomes.
System of Record and Administration. Health systems want to get into the risk business, but they probably don’t want to get into the claims processing business. Even if they want to handle all other aspects of care themselves, they can still use Oscar’s claims system on its own to make that part of the process easier.
Partners can essentially take advantage of these simple layers, or they can dial it up and get creative. For example, one system might design plans specifically for people with diabetes that incentivizes healthy eating, another might design a plan for people with sleep issues that comes with a free Calm subscription, Oura ring, and blue light glasses.
When the people providing the care are also the people paying for it, they’re incentivized to design plans that improve health outcomes and lower total cost of care over a patient’s lifetime. +Oscar gives them the tools to get as creative and specific as they want to be.
In that sense, Oscar is arming the rebels, like Shopify. There are smaller hospital systems across the country that are doing billions of dollars in revenue, who want to take risk and become value-based providers, but don’t have the tech or underwriting wherewithal to do it. Oscar can help.
Oscar wants to give all of them the tools that they need to make that transition, and build hundreds of insurance businesses custom designed for the populations they serve to take on the big, fee-for-service incumbents that dominate the industry today.
Putting Together the Puzzle
Health insurance in the US, as it stands today, is a mess. Expensive, confusing, misaligned.
But the incumbents have something that no startup can, which happens to be incredibly important in insurance: scale.
One argument against Oscar, and other health insurtech companies, is that insurance is insurance, and the big insurers are too tough to compete with. They’re too big. UnitedHealth is 73x larger than Oscar, having written $176.7 billion in direct premiums in 2020, good for a 14.1% market share.
If you’ve been reading this newsletter for a while, you know that that’s not a belief that I subscribe to. I’m more of a “software is eating the world” person.
In The Model of Everything, I wrote that, “After writing about NexHealth and now ScienceIO, I’m convinced that healthcare will see the kind of change in the next decade that fintech has in the last one.” A little over a decade ago, the banks were too big to compete with; now, fintech players are stealing meaningful market share. Today, the health insurers are too big to compete with, but Oscar is growing and stealing share.
Whether Oscar is ultimately able to disrupt health insurance and build a huge, profitable business comes down to three questions:
Is its technology useful in engaging and retaining members and giving them better health outcomes at a lower cost over their lifetimes?
Will hospital systems and other care providers partner with Oscar to capture the upside associated with better care?
Will those partnerships add up to the kind of scale that drives down Oscar’s costs, improves its plans, leads to better outcomes, and lets them compete head-to-head with the big insurers, even in the larger employer market?
The early signs are positive. Oscar’s members are more engaged. Oscar’s NPS looks more like a tech company than an insurance company. Before this last quarter, Medical Loss Ratio was improving steadily. Now, health systems are increasingly turning to Oscar in order to take on risk. In addition to successful launches with Cleveland Clinic and Montefiore, Oscar partners with large insurers like Cigna and HealthFirst. Now, they’re managing a serious Medicare Advantage book in addition to the large and growing individual book and a seedling small group book.
A decade in, the Oscar flywheel is really beginning to spin. It still requires some pushing, but the beauty of running a technology business is that once it starts spinning fast enough, it can eat everything around it much faster than expected.
As more healthcare systems start earning more profits by taking risk and aligning their incentives with members, competitors won’t have a choice but to switch. Oscar can partner with them to grab more of the individual, small group, and Medicare Advantage markets, and it can start going after large group (employer) insurance, the big prize.
To Mario, it’s just a matter of sequencing. Maybe you power smaller large group insurers first, or wedge in with Virtual Plans, in which Oscar Medical Group takes direct risk on outcomes, on top of a company’s UnitedHealth plan. Prove that businesses can save money downstream by working with Oscar. And then in the future, whether in five years or a decade, go head-to-head with the giants.
It’s as simple as building a world-class tech-enabled insurance business and then unbundling that tech and delivering it to hospital systems to let them take risk and share in the upside for the great care that they provide, and then leveraging the combined scale of Oscar and its partners to build a better and better health insurance business and tech platform until it eats all of health insurance from the bottom up.
Large groups are ultimately just large groups of individuals. The real bet that Oscar is making is that from the individual all the way up to the large groups, people expect a better experience than they’re getting. This happened in SaaS – the cringely-named “prosumerization of the enterprise” with consumer-quality enterprise tools like Slack and Figma. If Oscar can do the same thing to healthcare, even if it takes another decade, $1.5 billion will seem a cheap price to pay.
Thanks to Dan for editing, and to Josh, Mario, Jackie, and JoAnna for working with me!
How did you like this week’s Not Boring? Your feedback helps me make this great.
Loved | Great | Good | Meh | Bad
Thanks for reading and see you on Monday,
Packy

























This is incredibly well researched and written. Thank you for going through the effort.
As an insurance professional, we have now seen quite a few entrants coming in who are moving the needle, but I think there are some elements of insurance economics from which add to the complexity of the analysis. Ultimately, what are the economics that are going to drive the valuation? Is it insurance economics or SaaS/tech economics? The valuations for companies like Oscar and Lemonade where is the SaaS stratosphere. Much of the correction, is that investors are predicting that as much value as the technology these companies bring to the table, ultimately, they will NOT be able to capture that value in the same way traditional software companies can. This is because there are no winner-take-all dynamics at play. Making it easier for someone to buy and interact with insurance is a value creation exercise...but the COGS in the form of claims are unknown at the time of sale and they are leveraged (meaning with the wrong customer population, you can have losses that are multiples of what is budgeted). Because of this, there is not enough capital in the world to support the tail of the losses. So companies like Oscar will be dependent upon reinsurance indefinitely. Because of this, they can only carry poor loss ratios for so long before the costs of reinsurance escalate. Insurance is a great business at scale when the flywheel is positively spinning...but unlike other industries, the flywheel can spin in a negative direction. Long term success in insurance depends on short term profitability to secure less expensive reinsurance deals AND to grow book value to generate the secondary float income. These companies that are growing rapidly don't have any mechanism to the latter and it is the latter that has made State Farm and Allstate and Berkshire and Aetna and all of the other dinosaurs tech enthusiasts laugh at. But you cannot disrupt billions of liquid assets that support the premium volume they have. What investors see, and I think properly, is that these Insurtechs growth, fueled by their technology, could actually kill the companies. Investors are properly valuing these companies as insurance companies and not tech companies.
I do like what Oscar is doing. They are bringing needed value to the marketplace. Until they find a value capture mechanism, investors don't see a need to keep financing a capital burning enterprise, regardless of how much value they create. My $0.02
So Oscar is paying you?
Edit: so Oscar and Thrive are both paying you?!? This investment advice / marketing is blatantly designed to deceive the investing public.
Not ok guy!!