Ezra: The Quest to Kill Cancer
A Sponsored Deep Dive on Early Detection as a Cure
Welcome to the 964 newly Not Boring people who have joined us since last Monday! If you haven’t subscribed, join 204,865 smart, curious folks by subscribing here:
Today’s Not Boring, the whole thing, is brought to you by… Ezra
Ezra is on a mission to detect cancer early for everyone in the world. The company offers full-body MRI scans in order to catch cancer earlier to increase the odds of beating it.
I recently did an Ezra scan myself, and while it was nerve-wracking to face cancer, confirming that I’m cancer-free was a priceless relief. My scan took 60 minutes, but Ezra just received FDA clearance for the world’s first 30-minute full body MRI to screen for cancer. It’s faster, more affordable, and just as accurate thanks to Ezra Flash AI.
Book your Ezra scan and use the code PACKY150 to get $150 off.
Hi friends 👋,
Happy Thursday! Hope you had a great long weekend and that your summer is off to an excellent start.
Not Boring’s mission is to make the world more optimistic. On that quest, we’ve written about everything from fusion to AI-driven drug discovery. These are big, bold, sexy bets that, if successful, will make the world a fundamentally better place.
But sometimes, the solutions are simpler. Ezra, the subject of today’s piece, believes that early detection is the cure for cancer. It’s on its own mission to decrease the cost and increase the accessibility of cancer screening in order to catch cancer early, when it’s easier to treat. A world in which cancer no longer claims millions of lives annually would be a fundamentally better place.
Today’s essay is a Sponsored Deep Dive, and one of the ones I’m proudest to bring you in Not Boring’s history. In the spirit of not writing about anything I wouldn’t do myself, I got screened a few weeks ago, and I’m glad I did. You can read more about how I choose which companies to do deep dives on, and how I write them here.
Let’s get to it.
Ezra: The Quest to Kill Cancer
Let’s start in the future. Pick a year, say 2050.
In the year 2050, each time you step in front of the mirror in your bedroom, it runs a quick and dirty MRI on you. The MRI won’t be as high-resolution as something you would have gotten in a tube in 2023, but it doesn’t need to be. AI fills in the gaps and pulls signal from noise.
Most days – 99.9% of days – you don’t even remember you’re being scanned. There’s nothing to report, so your mirror reports nothing.
Very occasionally, though, it might notice enough of a change in your cells that it recommends a higher-resolution, localized scan on, say, your prostate, moves some things around on your calendar, books you an appointment, and summons your car to whisk you away to an imaging facility for a closer look.
The facility runs a prostate scan, AI flags the relevant parts, a radiologist reads them, and a doctor tells you the three words that used to be among the most devastating in any language: “You have cancer.”
They follow up, however, with words that have become commonplace: “It’s very early, the earliest stages of Stage 1, and we can cut it out.” Your car whisks you to a nearby facility where surgeons, armed with a precise, 3D map of your tumor’s location in the prostate, snip it out before it has the chance to spread. Minutes later, a doctor delivers the good news: “You are cancer-free.” The doctor prescribes a personalized immunotherapy to head-off the chance of remission. You go on living your life.
Unfortunately, this is not the world we live in today.
As it stands, cancer is the second-leading cause of death in the United States, behind heart disease, and the number of cancer deaths continues to grow annually.
According to the Institute for Health Metrics and Evaluation, 773,895 Americans died of cancer in 2019, up from 539,139 two decades ago. Numbers are cold, though; cancer is more personal. All of us know people who have, have had, or have died from cancer. My dad’s mom and my high school cross country coach both passed away from cancer, and I consider myself lucky that the list is so short.
Half of all men will have cancer at some point in their lives, as will one-third of women; half of all of them will detect it late.
Cancer is a devastating disease. It comes from inside of us, as our own cells turn on us and divide uncontrollably. “Cancer cells can grow faster, adapt better,” wrote Ezra Scientific Advisor Dr. Siddhartha Mukherjee in his Pulitzer Prize winning biography of cancer, The Emperor of All Maladies. “They are more perfect versions of ourselves.”
Cancer is particularly pernicious because as we devise cures to the diseases that might have killed our great-grandparents at a young age, cancer lies in wait, a final boss whose presence becomes likelier with age.
It’s particularly frustrating because it seems so simple to cure. There’s a lump. We can see it. We have robots and precision surgery, but we can’t just cut out the lumps?
There’s good news, however. We’re early on the curve towards that 2050 future I described.
“We have a cure for cancer. It’s early detection.”
If you spend any time with Emi Gal, the founder of cancer screening startup Ezra, you’ll hear those two sentences.
They’re the basis of the company’s mission – to detect cancer early for everyone in the world – one that’s personal for Emi: he’s at high-risk for skin cancer, and sadly lost his mother to metastatic colon cancer after she discovered it too late.
The numbers that back the words up adorn the company’s home page:
Ezra, which Emi founded in 2018, wants to make it easier and cheaper for more people to get screened for cancer, and for radiologists to interpret the results of the screens, in order to catch cancer early, when it’s most easily treatable. The bet is simple and profound: early screening and detection can lead to earlier treatment, which could save millions of lives.
Over the past five years, Ezra has screened over 5,000 people using a specialized 60-minute MRI running on 3 Tesla scanners (these are newer MRIs able to obtain high resolution images, faster), detecting cancer in 13% of them and non-cancer actionable clinical findings in 70% of them. I recently did the scan myself, and am happy to report that I’m cancer-free.
Today, the company is announcing its biggest leap to date: the 30-minute Full Body Flash scan, which cuts both the time and cost of getting an MRI to screen cancer in half. Ezra Flash, the AI powering the new scan, has recently received FDA clearance, enabling Ezra to launch the world’s first 30-minute Full Body MRI scan. The new scan is now available for booking on Ezra’s website.
In scanning, time is money. Ezra uses AI to decrease the time in the scanner, the time it takes radiologists to read scans, and the time it takes staff to write up reports, all in service of getting to the point where screening is cheap and ubiquitous.
Cheap and ubiquitous scanning, an unequivocally good thing, no? Not exactly.
This is a hot topic and very much up for debate. Friend of Not Boring Nikhil Krishnan recently wrote a piece, Why don’t we screen healthy people to catch diseases early?, that lays out the drawbacks of screening healthy people.
At the heart of the battle lies the issue of false positives – when a screen says you have something that you don’t have, prompting unnecessary and potentially harmful treatments. It’s a topic that’s come up time and again in my conversations with the Ezra team. They agree that false positives are a huge issue, they just don’t believe they’re insoluble.
The key, according to Ezra, is longitudinal screening: getting screened on a regular cadence to monitor changes as opposed to operating based on point-in-time measurements. Emi responded to Nikhil’s post with his own, On incidental findings, describing Ezra’s approach.
There’s no dispute, however, that catching cancer earlier increases survival rates. This holds true across every form of cancer: if you can kill cancer where it first takes root, before it spreads to other organs, survival rates increase anywhere from 2-11x.

The challenge is figuring out how to identify true positives while minimizing false positives, and dealing with the inevitable false positives in a way that first does no harm.
And that’s exactly what Ezra is working to do, alongside its world-class team of Scientific Advisors, including Dr. Daniel Sodickson, who invented parallel MRI, and Dr. Siddhartha Mukherjee, who literally wrote the book on cancer. They’re combining tried-and-true imaging methods with cutting-edge AI to see into our bodies more clearly than ever before.
As importantly, they’re making screening cheap and easy enough that more people can get screened early to establish a baseline, and continue to screen regularly throughout their lives to identify changes. Screening, like cancer, is not a static thing.
Cancer screening is a technology whose time has come, and one that Ezra will continue to improve with time. Today, we’ll cover the why, what, and how:
The Ezra Story. Emi’s personal journey to early cancer detection.
Inducing Demand with AI. How Ezra leverages modern tech to find cancer.
Confronting Cancer. Or, why I stopped delaying and got scanned.
My Ezra Experience. MRIs are kind of pleasant, actually.
My Results: Cancer Free. Don’t want to bury the lede; my results were negative.
Screening Out False Positives. How Ezra minimizes the risk of false positives.
Killing Cancer. Getting to a world without cancer.
By the end of the piece, I hope you’ll consider getting a cancer screening. I did it myself, and once I got over the fear of finding out, it was painless and ultimately reassuring. You can use the code PACKY150 on Ezra’s website to get $150 off your scan.
But first things first.
The Ezra Story
Emi Gal’s story is the modern entrepreneur’s story: make money in software, then put the resources towards a Good Quest.
Born and raised in post-communist Romania, Emi fell in love with computers after his mom saved up enough to buy a computer for him and his sisters. He learned BASIC at age 10 and started his first company at age 19 while still in college studying computer science and applied mathematics.
The company, Brainient, launched an interactive video ad server in 2009 that became the leading video ad server in Europe. His youthful success landed Emi on the cover of Forbes Romania’s 30 Sub 30 edition, for which he took this incredible photo:
In 2016, Emi sold the company to Teads and moved to New York, where he ran Teads Studios for two years before leaving to find a challenge he could work on for the rest of his life.
In Choose Good Quests, Trae Stephens and Markie Wagner call out curing cancer by name:
A hard quest is high-risk and operationally complex, with a low chance of success. Reversing aging, going to Mars, curing cancer, building a supersonic plane, creating AGI, or founding a new country — these are all hard quests, and most players attempting these quests will fail.
Early success in software provided Emi with the means to embark on his Good Quest: curing cancer. His Good Quest was also a personal one, sharpened by two formative experiences.
As a child, Emi developed hundreds of moles on his body, which put him at risk for skin cancer and in the dermatologist’s office for annual check-ups to screen for moles. He grew up living with the importance of regular screening.
Later, in 2015, a friend introduced him to Hospices of Hope, a Romanian non-profit that builds and operates hospices for terminally ill cancer patients. While skin cancer is visible and therefore easy to screen for, his conversations with patients and their doctors at Hospices of Hope helped him realize that “one of the biggest problems in cancer is the lack of a fast, accurate, affordable way to screen for cancer everywhere in the body.”
The question was how to solve that problem. Preventative cancer screens were expensive, often unpleasant, and potentially harmful, full of needles, biopsies, and false positives.
The answer came in the form of a 2018 study that Emi read while noodling on potential solutions: MRI.
In May 2018, a group of researchers published a study titled MRI-Targeted or Standard Biopsy for Prostate-Cancer Diagnosis in The New England Journal of Medicine. I’ll let them explain the issues with prostate screening at the time (emphasis mine):
Men with a clinical suspicion of prostate cancer on the basis of an elevated prostate-specific antigen (PSA) level or an abnormal digital rectal examination are typically offered a standard transrectal ultrasonography–guided biopsy of the prostate during which 10 to 12 cores are obtained. This approach is associated with the underdetection of higher-grade (clinically significant) prostate cancers and the overdetection of low-grade (clinically insignificant) cancers.
TechCrunch described the standard method more colorfully: “Typically, prostate cancer screenings involve a blood test for prostate-specific antigen, with a needle-through-the-rectum biopsy done if PSA levels are elevated.” Not fun!
Fortunately, the NEJM study found that, “The use of risk assessment with MRI before biopsy and MRI-targeted biopsy was superior to standard transrectal ultrasonography–guided biopsy in men at clinical risk for prostate cancer who had not undergone biopsy previously.”
In English, doing an MRI scan before sticking a needle in the rectum was superior both at avoiding the needle altogether when it proved unnecessary and at guiding the needle when a biopsy was required.
Emi read the study and in it discovered a path to a faster, more accurate, and more affordable way to screen cancer. So in 2018, he started Ezra, initially focusing on a subscription product that used MRI and AI to better screen for prostate cancer.
Let that early marketing image show that Ezra has been using AI since before it was cool. Specifically, Ezra found that its AI model was able to agree with radiologists on a data set from the National Institutes of Health.
The company was the first to ever receive FDA clearance for an AI to analyze prostate MRI images, and was able to offer annual 20-minute prostate scans for $999 per year. The seeds of the Ezra model were planted in those early days, centered on improving the speed, cost, and accuracy of screens:
Bulk MRI Time. Ezra buys MRI slots from existing imaging centers at a discount.
AI to Support Radiologists. Ezra’s models help radiologists identify issues more quickly.
Within six months, Emi moved beyond the prostate (which it still offers as a standalone screen for $750) to the full body, screening for 11 cancers in men and 13 in women in just one hour for $1,950. These scans cover organs that aren’t typically screened for cancer, and are complementary to existing screens like those for breast, lung, and skin cancer.
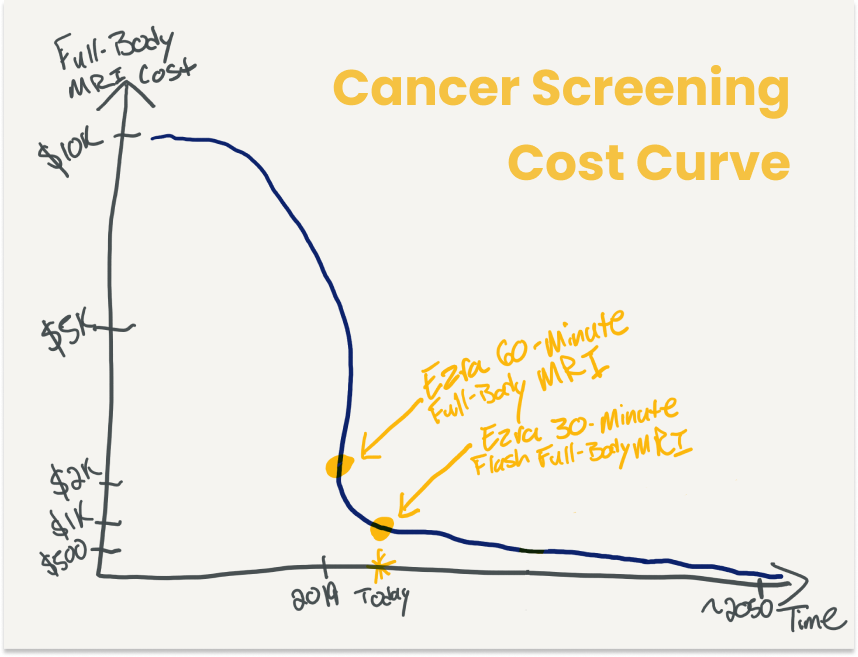
Since insurance doesn’t yet cover Ezra scans, $1,950 is still a significant out-of-pocket expense, but it represents a huge improvement over the prevailing $5,000-$10,000 price of a full-body MRI.
With lower costs comes the ability to do more regular screens. With more regular screens – longitudinal monitoring – Ezra can minimize false positives by comparing scans instead of overreacting to a one-off scan. To make longitudinal monitoring more effective, Ezra has been direct-to-consumer since the beginning because, as Emi told me, “We want to be a consumer’s partner in screening, with a direct relationship where you store and analyze all of your data over time.”
This stands in contrast to the way it’s currently done, where data is stored on physical CDs that patients need to physically carry from one location to the next if they change doctors or move cities. As evidence, the key chains at the facility where I was screened were CDs.
In late 2019, Ezra raised an $18 million Series A led by Rick Heitzmann at FirstMark Capital. By 2021, Ezra had completed 1,000 screenings. Now, just two years later, it’s done over 5,000 screenings.
To date, Ezra has detected cancer in 13% of the people it’s screened and identified actionable clinical findings in a total of 70%.
Again, though, numbers are impersonal and cancer is personal. One Ezra client discovered a brain tumor that turned out to be glioma, a malignant but potentially slow-growing tumor that doctors told him could have taken 5-10 years to find otherwise. After a successful surgery, the client quit his job and started a PhD program at Columbia to work on cancer detection.
There are many such stories. As a reminder of the company’s mission to detect cancer early for everyone in the world, a #morelife wall is displayed in Ezra’s New York office - real stories of members who discovered life-saving information through their Ezra scans.
From the beginning, Ezra has been focused on creating more stories like that by bringing screening to more people with the belief that screening is the cure for cancer, an idea Cleo Abram captured brilliantly in her recent Huge* If True video:
Ezra is still very early in its mission. 5,000 people is a small fraction of the billions of people worldwide who might benefit from cancer screening.
To get from here to there, Ezra plans to induce demand with AI.
Inducing Demand with AI
In April, I wrote a post called Intelligence Superabundance about induced demand and Jevon’s Paradox – related ideas that describe increases in demand based on increases in supply and efficiency, respectively. Build more roads, get more traffic. Make more efficient steam engines, use more coal. I argued the same thing would happen for intelligence with the rise of AI.
Turns out, it’s already happening in cancer screening.
Later that week, I talked to Dr. Dan Sodickson, the Chief of Innovation in Radiology at NYU and Ezra’s Chief Scientist. Dr. Sodickson is a legend in the imaging space. At the end of his Harvard/MIT MD/PhD program, he became fascinated with a question: why aren’t scans faster?
MRI scanners at the time were like fax machines, with a single detector gathering one data point at a time in a slow scan of the body. Or, since Nvidia is hot this week and we’re talking AI, they were like the data-gathering equivalent of CPUs, powerful but single-threaded. What if you could use multiple detectors at once and then triangulate your way to a complete picture?
That’s what Sodickson did, inventing parallel MRI, “the use of radiofrequency (RF) coil arrays to acquire MRI data in parallel rather than in a traditional sequential fashion, thereby enabling imaging at previously inaccessible speeds.” Parallel MRI is like a GPU, a multi-threaded data gatherer. “The time savings are similar,” Dr. Sodickson told me when I floated the analogy, “The same is true whether you’re performing computations or gathering data.”
Parallel MRI works because of computer algorithms. The scan actually generates less data than sequential MRIs, but can generate complete images by stitching them together with algorithms.
Since then, Sodickson’s entire career has been a quest to answer that original question – why aren’t scans faster? – using the best technology available, as evidenced by the breadth and volume of his publications over the past 27 years.
Sodickson’s mission, and the progress in much of biomedical imaging during his career, has centered around doing more with less: generating higher-quality images with less data to go faster. That approach has four main benefits:
Raw Healthcare Costs. The quicker the scan, the lower the costs.
Patient Comfort. Patients appreciate being in the tube for less time.
Movement. People and their organs move, so faster means higher accuracy.
Accessibility. Faster and cheaper mean that more people can get screened.
Sodickson admitted that “MRI right now isn’t the most accessible of technologies,” but he’s optimistic that AI can help. This is where we bring it back full circle to Intelligence Superabundance: he told me the piece I wrote described exactly what was happening in his field.
The ideal state of screening would be to be able to screen everyone, regularly, cheaply, and quickly, while minimizing false negatives and especially false positives, like in the 2050 scenario up top. That’s not the state of the world today for a number of reasons, which can be boiled down to two: cost and capacity.
Cost. Historically, MRIs have been too expensive for most people unless insurance foots the bill, which it typically doesn’t for preventative screening. That means fewer people screened, but it also means that even the people who do get screened probably can’t get screened with a regular enough cadence to build up a longitudinal history, which would help rule out many of the false positives identified in one-off exams.
Capacity. Say you’re able to lower the cost, or at least to convince insurance to cover it. Then, you have two problems with capacity. First, MRI tubes are big, expensive machines operated by skilled professionals. More demand would overwhelm current MRI capacity. Second, radiologists are also in high-demand, and more scans would mean more time reading scans (a scan for each different body part may be read by a different radiologist in a process that can take hours) and writing up or dictating reports (can take 90 minutes) .
Of course, over time, you could spend the money on more tubes and educate more radiologists, which would just increase cost. So it all comes down to cost, and as Sodickson explained to me, cost is a function of scan time and radiologist time.
AI can help on both fronts. It can increase scan volume and help radiologists process the increased wave of scans. More efficient screening and reading leads, Jevon’s Paradoxically, to more screening and reading.
Early warning scans, long a problematic holy grail in imaging, might finally be practical. When I asked him why he teamed up with Ezra, Sodickson told me, “I’d been reading the tea leaves in radiology, and seeing more things that would allow us to move to early warning. People were starting to work on more accessible machines and bring AI in to do triage. I felt like it was time to rethink longitudinal monitoring.”
Ezra currently uses AI in three main ways to induce longitudinal monitoring demand:
Faster MRI Acquisition
AI-Assisted Radiology Reads
Report Creation
All three fit together – faster, cheaper scans require better ways to handle the outputs – so we’ll touch on each of them.
Faster MRI Acquisition
Ezra recently received FDA clearance on its newest AI offering: Ezra Flash AI. The technology allows Ezra to decrease scanning time by 50% without decreasing image quality (the AI removes noise and improves the quality of accelerated MRI scans).
Ezra Flash AI is trained to understand what noise looks like in MRI images. That means that they can do faster scans by pushing parallel MRI to its limits and remove the noise in the images without removing any of the important data that would help identify a pathology, as seen in the video above and the images on Ezra’s website.
For clients, that translates into scans that take half the time (30 minutes) and cost nearly half as much ($1,350). It’s the world’s first 30-minute full body MRI on the market.
AI-Assisted Radiology Reads
Ezra also uses AI to help radiologists read and compare scans, and to more precisely target where to biopsy. A couple of years ago, the company received FDA approval for Ezra Prostate AI - the first of its kind.
Prostate cancer can be slow-moving, which means that even when it's detected, radiologists may just want to monitor how it progresses over time before deciding to treat it. The challenge is, those changes can be hard to detect – Sodickson told me that radiologists often put the two images on a screen and flicker them back and forth like a flip book to pick up changes.
Ezra Prostate AI segments the whole prostate and helps radiologists pick up on lesions. As Emi described it, if radiologists measure the lesion volume like a cube by taking three measurements on three axes, Ezra Prostate AI measures thin slice by thin slice for greater accuracy. It’s able to help radiologists detect changes over time by providing more accurate measurements. It also produces a 3D image that medical professionals can twist and turn to monitor progression and determine exactly where to biopsy when a biopsy is needed.
Ezra is currently training the AI to bring the technology to more organs, and is expecting to have full-body coverage as soon as next year.
If Ezra Flash AI means cheaper, faster scans and therefore more scans, then technology like Ezra Prostate AI helps radiologists handle the increased volume with more accuracy.
Report Creation
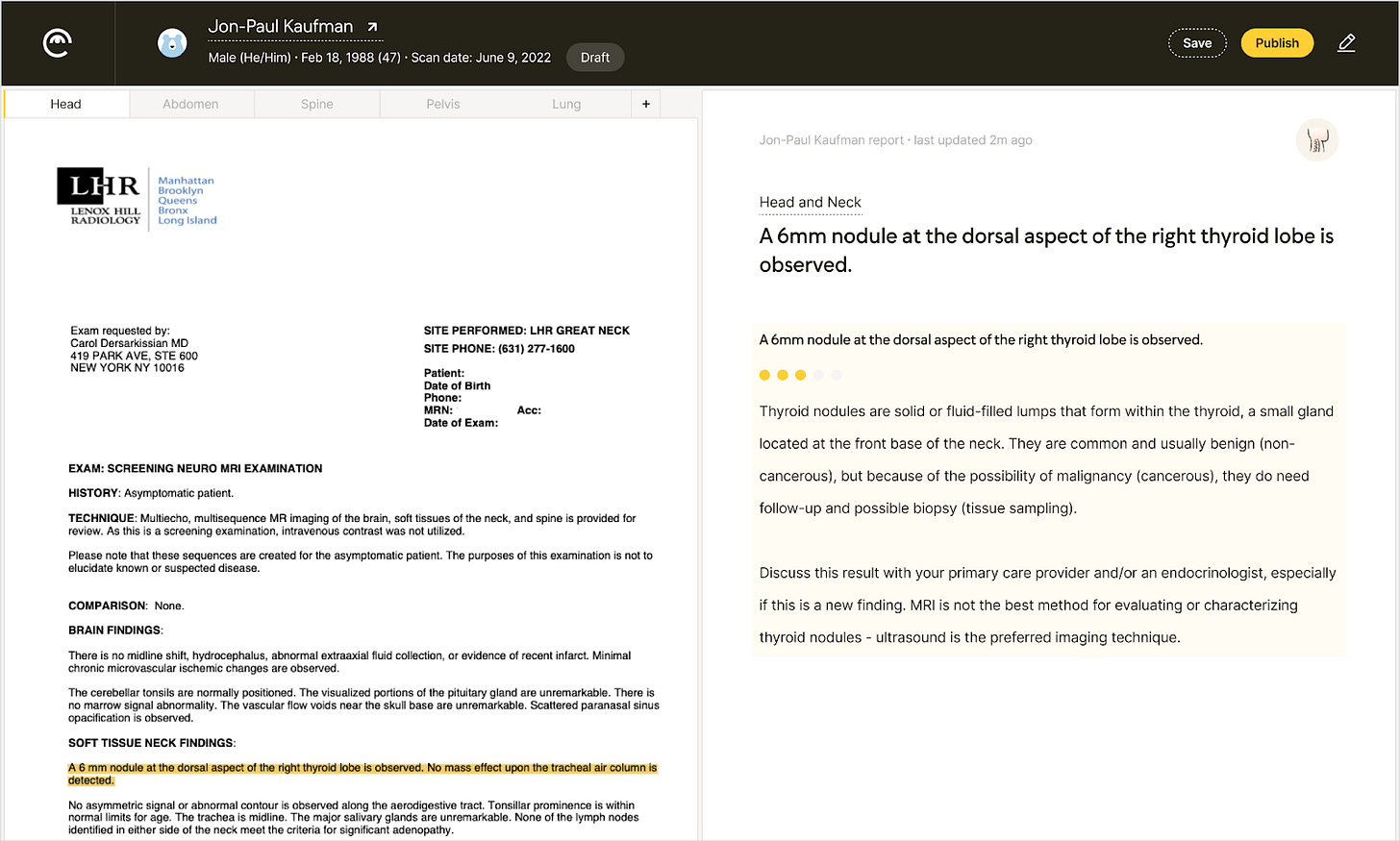
Finally, Ezra Reporter AI is a ChatGPT-like tool that turns radiology reports into readable reports that a lay person can understand.
Way before the launch of ChatGPT, Ezra had manually compiled a database of over 5,000 findings to train their AI model. Now, the model automatically compiles a report based off of the scans and radiologist readings, and sends the report to medical professionals who tweak and approve them. It takes what used to be a manual, 90 minute process down to five minutes, and means that Ezra can deliver reports to members in 3-5 days instead of 7-10 days.
Ezra Reporter helps bring down time spent by medical professionals, which lowers costs for consumers and, crucially, reduces the time spent waiting for results.
Taken together, Ezra’s suite of AI products means faster, cheaper, more accurate, more actionable, and more understandable scans and readings. By unlocking supply (30-minute scans means that twice as many people can get screened at every facility), they should create more demand for screens, help radiologists manage the increased volume, and support the company’s internal medical providers in spinning out reports. Induced demand, and the tools to handle it.
All of the technology, however, is in service of the screening experience and results.
To make it more concrete, I’ll share my experience with Ezra. Turns out, the hardest part of the whole thing was confronting my mortality and deciding to do the scan in the first place.
Confronting Cancer
It’s not good, I know, but I have not been to the doctor for a checkup since I moved to New York in 2009.
On the one hand, if a disease falls in my body and no doctor is there to see it… all good, right?
On the other, there’s a little bit of existential dread that slowly accumulates over time. The longer I don’t go to the doctor, the less I want to go to the doctor, because the more I think there’s likely to be something wrong when I do.
When I’ve allowed my brain to go there over the years, I viewed myself as a kind of Schrödinger's cat: neither healthy nor unhealthy, or both healthy and unhealthy, until an observer observes.
I’d still have no idea what was going on in there if it weren’t for this newsletter.
A couple of years ago, I signed up for Fount because a) I wanted to get my energy back, and b) I needed to do the program if I was going to write about it. I was excited about the whole thing – the blue light glasses, the Oura ring, the diet and meditation, the workouts – except for one part: the blood test. At the beginning of the program, and every 5 weeks thereafter, I’d need to get my blood drawn so that the Fount team could understand what was happening in my body and personalize my plan. That part worried me.
I wasn’t worried about the needles; I was worried that the results would come back and I’d hop on a call with my coach, who would tell me, “I’m really sorry but it’s just a bunch of gerbils running around in there,” or something, “When’s the last time you went to a doctor?”
Turns out, I was mostly fine, but the test discovered that I was anemic, among other minor things. Over the next few months, we fixed the anemia. I ended up with a bunch more hemoglobin and a little more peace of mind.
Not full peace of mind, though. Back in high school, when I ran cross country and track and therefore couldn’t smoke cigarettes with the cool kids, I dipped with the other runners who couldn’t smoke cigarettes with the cool kids. After practice, we’d drive around and crack open a can of Skoal; on Friday nights, we’d go to the movies and indulge in popcorn, soda, and Skoal.
I noticed little bumps in my mouth then, but I was young and invincible and thought they’d just go away. Another lifetime later, they’re still there, and with them, a little nagging voice in my head that maybe they’re cancer. Every time I run my tongue across the inside of the bottom of my mouth, part of my brain flashes a little image of me in jaw-removal surgery. That image has been there for a long time, and I’ve gotten used to it, but when I had kids, it became particularly scary. What if my kids had to grow up without a dad because of some youthful tobacco indulgence? What if I couldn’t see them grow up?
But of course, that thought was too terrifying to confront, so I just kind of shoved it into the depths of my brain as hard as I could and hoped for the best. Then, a few months ago, Fount’s CEO, Andrew Herr, introduced me to Emi. Emi was interested in a Not Boring piece about Ezra, and Andrew (my health guru) was a proponent of the product, so we chatted.
As I learned more about Emi’s story and about Ezra, about all the things you’re reading about in this piece, I knew it was a story I wanted to tell. It’s not often I have a chance to save lives with a Deep Dive. But that also meant something pretty uncomfortable: I’d need to confront that lingering fear and get a cancer scan.
My Ezra Experience
Booking the scan is easy. I went to the Ezra site and picked a location, date, and time.
Then I waited.
The waiting was hard. The two weeks between booking and scanning felt longer than a normal two weeks. Those quiet fears got a little louder. Like an unwitting Stoic, I had to confront death in the early morning and late night hours when I didn’t have other things to occupy my mind.
In preparation, I took Ezra’s Risk Assessment, a 5-minute quiz based on the Harvard Cancer Risk Index, to gauge my pre-test probability of having cancer. Whether or not you get scanned, I recommend taking the assessment: it’s useful to know your risk level, and the questionnaire serves as a good checklist of things to do and not to do.
I definitely eat processed meats more than 3 times per week, for example, and should probably stop doing that…
And if you use tanning beds, stop. The binary wording of that question - Have you ever used a tanning bed or sunlight? – suggests that it’s not a good thing to do.
Fortunately, my overall risk came out low: 18/100.
My highest risk category is for skin cancer (45/100), which as a half-Irish guy who spent summers lifeguarding on the beach checks out. Nothing I can do about that one now, but the test did return some lifestyle recommendations:
You can take my salt over my dead body, but I can eat less processed meat and more tomatoes. Plus, the risk assessment did calm my nerves a bit. Still, I had to get scanned to know for sure.
Finally, on a Friday morning in early May, I hopped in the car and drove up to Carnegie Hill. I parked, walked up the block, found the location, took a deep breath, and went inside.
Ezra doesn’t operate its own locations; it works with a network of hand-picked imaging centers across the country to do the MRI scans. They have 16 partner facilities in 6 cities (New York, San Francisco, Los Angeles, Miami, and Las Vegas). But Ezra clients get VIP treatment. When I walked up to the front desk, instead of handing me forms to fill out, they told me that they already had all of my information and asked me to take a seat.
When the person doing my MRI called my name a few minutes later, he walked me into the changing area and told me he’d give me a gown to wear during the scan. As I was thinking through how to walk down the hall without mooning poor passersby, he checked his notes and saw that I was with Ezra. Instead of an assless hospital gown, he grabbed me a fresh pair of Ezra pajamas and told me he’d wait outside while I changed into them.
Then a quick bathroom break, then the MRI room.
I’ve never done an MRI before, but I’d heard that it could be both claustrophobic and boring. I actually enjoyed it: an hour with absolutely nothing to do but close my eyes and relax. (I just missed the 30-minute Flash MRIs by a couple weeks.)
My plan was to meditate for the full hour, longer than I’d ever gone but I had nothing else to do. I pictured myself, enlightened and cancer-free, practically floating out of the imaging facility. As soon as I got in there, though, the MRI tech disavowed me of that notion.
He told me that we’d be doing three sessions of roughly 15 minutes, 15 minutes, and 20 minutes respectively, with short breaks in between. I was not allowed to fall asleep. And every few minutes, the machine would tell me to take a deep breath, hold it, and then let it out quickly. It would be loud, he warned, and asked me if I wanted headphones. I did. He asked what kind of music I wanted. I chose classical. If I couldn’t meditate, maybe I’d get smarter listening to the highbrow stuff.
With the warnings out of the way, the tech strapped me in, put a blanket over my legs (the MRI likes it cold), locked a cage-like thing over my head, and hit a button to roll me into the tube. I confirmed that I was good, and we got started.
When I’d heard that MRIs were loud, I’d always imagined a constant thrum. That’s not what it was like. A range of sounds shot out of various parts of the machine at inconsistent intervals and for inconsistent lengths of time. It sounded like it when Dev and Maya put on concerts.
Only once I’d spoken to Emi afterwards did I realize what was happening.
When you enter the MRI (Magnetic Resonance Imaging) machine, a powerful, 3 Tesla magnet aligns the spins of hydrogen protons in your body's water molecules. The loud noises are created by the gradient coils in the machine, which are used to alter the main magnetic field on a smaller scale for image creation. These coils create a changing magnetic field, which results in the coils physically moving or vibrating, causing the loud, inconsistent sounds.
The machine introduces heterogeneity via radiofrequency (RF) pulses to disrupt the alignment and flip the protons by degrees. Then it cuts them off to remove the interference. When the RF pulse is turned off, the protons "relax" and realign with the main magnetic field. As they do this, they emit a signal that the machine detects and uses to create an image. The rate at which the protons return to alignment, known as relaxation time, varies depending on the type of tissue, which helps differentiate between different types of tissues in the resulting images.
Finally, the MRI machine uses all the signals from the protons to create a detailed, cross-sectional picture of the body, which can show differences between normal and abnormal tissues to a trained eye (or AI).
Each time I slid in and out, the tech adjusted my smock, signifying that we’d be hitting different parts of my body with RF. In all, the scan hit my head and neck, spine, abdomen, and pelvis.
By the last session, the time flew by, and when it ended, I was almost bummed to head back into the fray. I changed back into my street clothes, kept my Ezra PJs, got in the car, drove home, and waited for the results.
My Results: Cancer Free
I got scanned on Friday, May 12.
Over the next few days, a few things happened behind the scenes over at Ezra:
AI Image Processing: 30 minutes
Radiologist Reading: 2-3 radiologists (neuro, body, and CT radiologists) review the scan, so this is the chunkiest piece of the process time-wise, and can take a couple days.
AI Report Generation: 5 minutes
Medical Provider Review: 5 minutes, unless there are tweaks, which can take ~15-30
All told, the process takes 3-5 days instead of the traditional 7-10, which is important when each day waiting feels a lot slower than a normal day.
Then on Wednesday, May 17, the email hit my inbox.
Remember when you were waiting to find out if you got into college, and a letter or email arrived, letting you know that inside awaited your future? Sweaty palms, audible heartbeat. That’s what it felt like clicking “View my Ezra Report.”
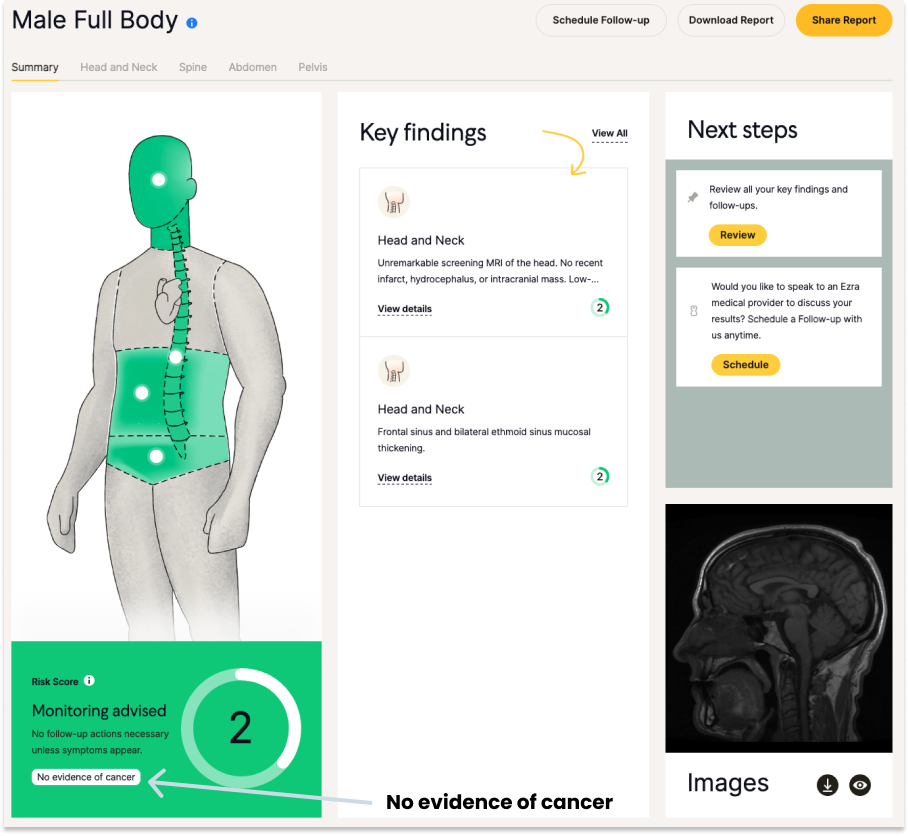
As soon as the page loaded though, I was hit with a flash of green, which I thought was a good sign. My eyes scanned the page furiously until I found it: “No evidence of cancer.”
I’d steeled myself against the idea that it would find something, and that because I was asymptomatic, it would probably be early and local, and so we would just cut it out and move on. Reading “no evidence of cancer” felt inaccurate for a minute. I clicked around to confirm that I wasn’t missing something. When it sank in, it was just a huge relief.
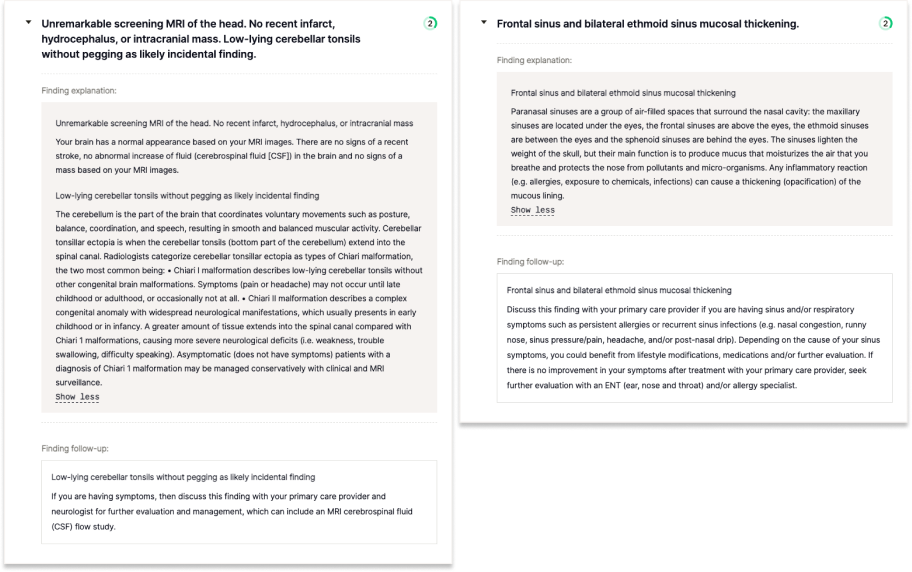
The scan uncovered a couple of things – “Low-lying cerebellar tonsils without pegging” and “Frontal sinus and bilateral ethmoid sinus mucosal thickening” – but the AI-generated report explained each in plain English:
Everything else, it told me, was “unremarkable,” a description of myself I accepted particularly gladly in this situation. This thing that had been gently gnawing at me – the idea that I probably had at least a little cancer – disappeared. This is, at the end of the day, what Ezra provides - peace of mind.
I’m not a medical professional and can’t offer medical advice. Talk to your physician and do your own research before deciding whether to get scanned by Ezra or another provider. As a consumer, though, I will say that I’m really happy I got screened and plan to do it regularly from here on out. Now that the cancer bogeyman is gone, I might even go to the doctor.
I’m sharing my experience because I hope that it makes you consider getting screened. It’s useful for the peace of mind, but even more valuable if it discovers something early, when it can be treated more easily and with a higher likelihood of survival.
Screening Out False Positives
While my test came up negative, the real danger with early screening is that it might turn up false positives, which can lead to high costs at best and procedures that might do more harm than good, at worst.
I didn’t fully appreciate when I set out to write this piece that I was wading into something of a war. Recently, for example, the US Preventive Services Task Force began recommending that all women begin mammography screening at age 40, down from age 50 previously, inciting backlash from those who believe that screening actually results in a net loss of life.
Nikhil’s piece, Why don’t we screen healthy people to catch diseases early?, is a clear-eyed look at what’s become an almost religious issue.
I highly recommend that you read both Nikhil and Emi’s pieces to get a more complete picture of the false positive issue. Dr. Peter Attia gives a good breakdown here, highlighting traditional MRIs’ high sensitivity and low specificity, which may mean that they’re good at not missing cancers, but come with a lot of false positives. He also covers the fact that software is helping MRIs reduce false positive rates.
That’s the approach Ezra is taking – using software to reduce false positive rates – and pairing that with a protocol that minimizes the downsides of false positives when they do occur.
I asked Emi what they would have done if they had found something that looked like cancer, and he told me that the next steps would likely have gone one of two ways:
Recommend that you monitor and return for a scan in a few months or a year.
Recommend a follow-up diagnostic scan that includes contrast to find out if it’s malignant, which will rule disease in or out. If it’s benign, they’ll recommend that you monitor it over time. If it’s malignant, only then will you undergo more invasive, and potentially harmful tests.
That’s one of the things that surprised me in my conversations with Emi and Dan. Both said that in many cases, if they find a cancerous tumor in the prostate, for example, the recommendation may not be to immediately go under the knife, but to continue monitoring it. Often, what matters is the rate of change, and not the existence of the tumor itself. If a client comes back for another scan in six months and nothing has changed, Ezra and the medical professionals it works with may simply recommend continued monitoring.
Ideally, though, as was the case with my scan, the first screening won’t find anything at all, but will establish a baseline. The next time I get screened, Ezra’s AI can compare my new scans with the old ones to see if anything’s changed, and flag any changes, no matter how small, to a radiologist for further review.
That’s the goal here: to make scans cheap, easy, and accessible enough that people begin to view them as a routine part of their medical care in order to build up a more accurate picture of what’s going on in their body over time. That, according to Ezra, is the path to killing cancer.
Killing Cancer
Screening isn’t the sexiest way to kill cancer.
Throughout the history of cancer treatment, macho would-be-cures like radical mastectomies, high-dose chemotherapies, autologous bone marrow transplants, and peripheral stem cell transplants have grabbed the lion’s share of excitement and funding. At Not Boring, we’re certainly excited about and investing in the next generation of potential cures, including immunotherapies.
The most important thing isn’t the novelty or force of the cure, however, but whether or not it works.
Writing this piece has made me confront a couple of things. My mortality, for one. As importantly, though, it’s illuminated the fact that the flashiest thing isn’t always the best thing. We all want a pill that we could take to protect ourselves from the devastating effects of cancer. That’s the kind of thing that we’d give top billing in the Weekly Dose of Optimism. But until that pill arrives, spending time in an MRI machine might be the best medicine we have.
That’s not to say screening can’t be sexy and isn’t evolving quickly.
Using AI to bring screening time down from 60 minutes to 30 minutes without sacrificing accuracy is a big step forward in convenience and cost, and using AI to help radiologists read scans more quickly and accurately will help them handle what is hopefully a deluge of screens.
And screening is only going to continue to improve from here. In my conversations with Dan and Emi, it really felt like the pace of improvements were picking up.
Emi described a coming shift: from creating images sharp enough for radiologists to read, to creating images designed to deliver only the data that an AI would need to flag something for further scanning.
Dan made a similar point, and one that’s interesting to think about in the context of AI more broadly. Not only does AI change what we’re able to do with the data we get from our current machines, it changes the kinds of machines we need to build and the type of data we need to gather in the first place.
If the history of MRI to date has been a race to stronger and stronger magnets (the reigning champ is 7 Teslas), then the next leg is about how small and portable we can make them without sacrificing results. He’s noticed a race to the bottom in the last few years, as imaging professionals have asked, “Can I make a 64 millitesla MRI?”
That might lead to a world in which your bra monitors for breast cancer and your hat checks your brain. Maybe, sometime around 2050, the world I imagined up top might be a reality.
For its part, Ezra is continuing to launch AIs that push MRIs down the cost curve. It hopes to develop a 15 minute scan that would cost around $500 in the next couple of years, putting cancer screening on its own Moore’s Law-like curve.
As cancer treatments improve simultaneously, I hope the combination of earlier detection and better treatments combines to make a cancer diagnosis as benign as cataracts. Hopefully, one day in our lifetimes, cancer will join tuberculosis, pneumonia, and polio in the growing list of once-fatal diseases that we’ve managed to overcome. That day can’t come fast enough.
Key to it all is building up your own history so that you can detect cancer early. If you want to try Ezra, you can book here and use the code PACKY150 for $150 off your scan.
Thanks to Dan for editing, and to Emi, Dr. Sodickson, and the Ezra team for sharing their insights and letting me tell the Ezra story.
That’s all for today! We’ll be back in your inbox tomorrow AM with the Weekly Dose.
Thanks for reading,
Packy
























Immensely interesting. The article educates, expands perspective, and may ultimately save lives. And thank
you for the links to additional information.
Great article. Early detection is one of the low-cost, high effective solution possible for solving the menace of cancer